Gut health and the immune system
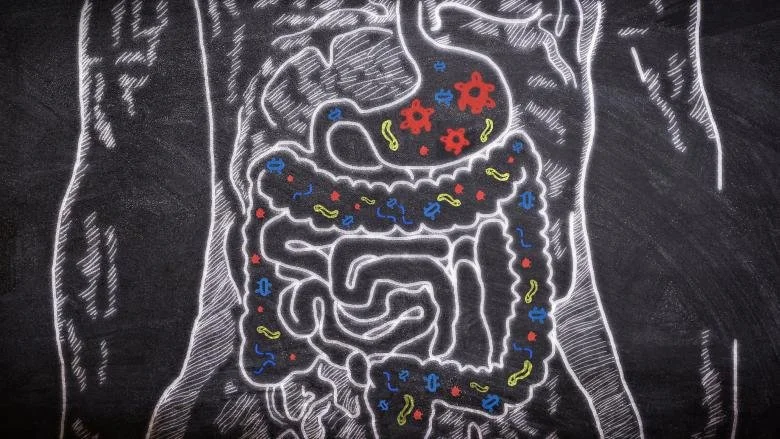
Approximately 70% of our immune system can be found in our gastrointestinal tract. As a result, the gut is our first line of defence against foreign invaders (e.g. viruses and toxins). Gut-immune interactions are complex and there is still much to uncover in this area of science, but research shows gut microbiota (the collection of microbes in our gut), and certain substances they produce (known as metabolites), play a key role in modulating their host’s immune response and protecting them from foreign invaders. These microbes and their metabolites communicate with immune cells in the mucosal lining of the gut, triggering the release of antibodies to fight off pathogens and protect against infection.
Immune cells in the gut are connected to a broad network of immune cells throughout the body, including the nose, lungs, and skin. Through this network of lymphoid tissues, it is thought that the gut microbiome helps to protect the body from systemic infection as well as gastrointestinal infections.
The immune system evolves throughout life, but recent research has highlighted the importance of the first three years of life in the development of the gut microbiome and, consequently, a healthy immune system. We now know that colonisation of gut microbiota begins when infants travel through their mother’s birth canal, meaning the microbiomes of infants born by caesarean can initially look very different to those born vaginally. However, studies show this colonisation continues throughout infancy and can be influenced by factors such as mother’s milk (e.g. breast milk contains beneficial bacteria and prebiotics to feed gut microbes), diet and environment.
Research suggests the development of allergies and eczema in children may be connected to low microbial diversity in early life. This altered development of an infant’s microbiome may result in an immune system imbalance, leading to overactivation of T helper 2 (Th2) cells, which is associated with onset of allergies.
The complexity of this field of science is made even more so by the fact we are all totally unique. Have you ever wondered why some people get lots of colds while others barely ever catch anything? Or some people endure weeks of symptoms fighting off a virus while others are rid of it in just a couple of days? Virulence factors of pathogens are known to play a part in this, but it turns out our individual response to infection can also be influenced by our microbiome (including the colonies of microbes in the mouth and lungs), and genes (which can modulate the outcome of infections or even stop us from getting some illnesses in the first place). For example, according to a 2016 study, some lucky people (around 20% of the Caucasian population) have a genetic mutation that protects them from norovirus.
Top tips to support gut health and immunity:
Eat 30+ different plant foods a week – These foods are packed with fibre and nutrients and eating 30 different types has been shown to create a more diverse microbiome (which can support immunity and reduce inflammation). 30 may sound like a lot but this includes fruits, vegetables, wholegrains (e.g. oats, brown rice), legumes, herbs, spices, nuts and seeds, so should be achievable for most people. Eating a rainbow of fruits and vegetables is also the best way to ensure your diet is rich in polyphenols, which have strong antioxidant properties and anti-inflammatory benefits. They also act as prebiotics, feeding beneficial bacteria in the gut.
Eat fermented foods daily - Foods such as live yogurt, fresh sauerkraut, and kimchi, and drinks such as kefir and kombucha, contain beneficial bacteria to support a healthy microbiome.
Include glutamine-rich foods in your diet - Glutamine is an amino acid that plays a key role in maintaining normal gut barrier function. Eating glutamine-rich foods regularly (e.g. fish, dairy, eggs, soybeans, red cabbage, nuts and beans) is a good way to ensure sufficient amounts and support healthy gut function.
Manage stress with yoga or meditation – Our modern environment is a stressful one. Stress impacts the microbiome and effectively ‘shuts down’ digestion by activating the sympathetic nervous system or ‘fight or flight’ response, which can lead to digestive issues. Yoga and meditation are both proven stress management techniques and are known to support gut health.
Exercise regularly – Exercise is proven to have a positive impact on the microbiome. If you can exercise outside in nature, then even better - this will provide natural support for the microbiome by exposing you to different microbes. However, be mindful that much vigorous exercise may invoke a stress response, which can have a negative effect on the diversity of our gut microbes.
Aim to get 7-9 hours of sleep – Insufficient sleep has a negative impact on the gut microbiome and immune system. Listen to your body - you may find you need more sleep for a while after an infection/illness.
Avoid ultra-processed foods – Highly processed foods (e.g. white bread, crisps, pastries, fried chicken etc.) are often low in fibre and high in sugar, salt and saturated fat, which can have a devastating effect on the gut (and general health).
Limit alcohol – Alcohol is a gut irritant linked to several gastrointestinal complaints including IBS-like symptoms. It is best to limit alcohol it if you are aiming to support gut health.